Frozen Shoulder Treatment
Free yourself from the suffering
Get professional, accurate and evidence-based treatment for your shoulder pain
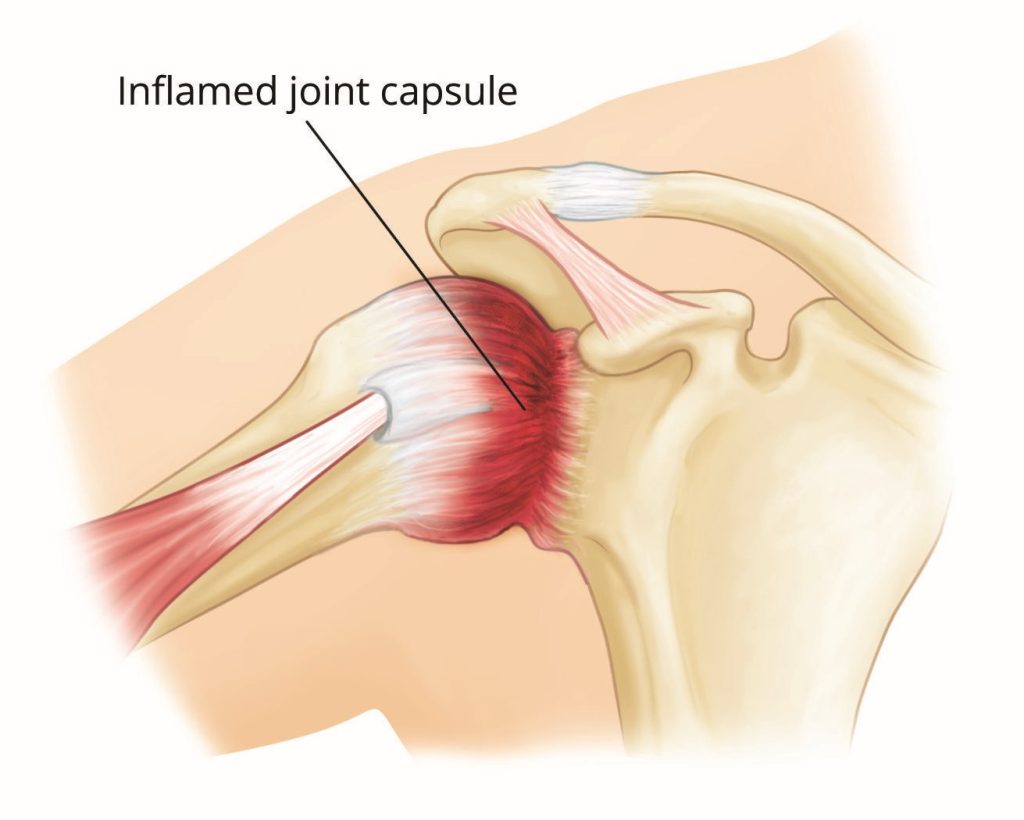
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by stiffness and pain in the shoulder joint. Over time, it can significantly limit your range of motion, affecting daily activities. Here’s everything you need to know about this common shoulder ailment.
Frozen shoulder occurs when the shoulder joint capsule thickens and tightens around the shoulder joint, restricting its movement. The condition typically develops gradually over time and can progress through three stages: the freezing stage, the frozen stage, and the thawing stage.
Risk Factors For Frozen Shoulder
Certain factors may increase your risk of developing a frozen shoulder:
- Age: Most common between the ages of 40 and 60.
- Gender: Women are more likely to develop frozen shoulder than men.
- Medical Conditions: Diabetes, thyroid disorders, heart disease, and Parkinson’s disease are associated with an increased risk.
- Immobilization: Prolonged immobility of the shoulder due to surgery, injury, or other conditions can lead to frozen shoulder.
Sign & Symptoms
Frozen shoulder typically presents with the following symptoms:
- Pain: Gradual onset of pain in the shoulder, often worse at night.
- Stiffness: Progressive stiffness that limits the range of motion in the shoulder.
- Difficulty with Daily Activities: Tasks such as dressing, reaching overhead, or even lying on the affected side become challenging.

Stages of Frozen Shoulder
Freezing Stage
Pain increases gradually, and range of motion starts to become limited.
Frozen Stage
Pain may reduce, but stiffness becomes more prominent, severely limiting shoulder movement.
Thawing Stage
Gradual improvement in range of motion as the shoulder slowly returns to normal.
Treatment Options for Frozen Shoulder
Treating frozen shoulder involves a combination of non-surgical, interventional injection and surgical methods, tailored to the severity of the condition and the stage at which it is diagnosed. The term “Frozen Shoulder” encompass a broad spectrum of different shoulder conditions such as Adhesive Capsulitis, rotator cuff muscle injury, tendinitis and tendinopathy and shoulder bursitis. Because of this, a thorough history taking and physical examination, aided by imaging study such as ultrasonography and MRI, is crucial in getting the accurate diagnosis thus providing effective treatment.
Here, we have outlined a step-by-step approach for the treatment of frozen shoulder.
Step 1: Conservative Management
This involves proper rest of the shoulder, regular physiotherapy and oral medications.
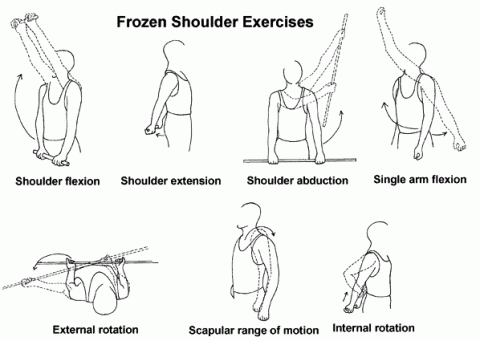
- Physiotherapy is the cornerstone of frozen shoulder treatment and focuses on restoring mobility through targeted exercises. A physiotherapist will guide you through a series of exercises designed to improve range of motion, strengthen shoulder muscles, and the use of heat and cold therapy to ease pain and inflammation. Physiotherapy is most effective when started early and continued consistently. As the shoulder gradually improves, the exercises become more intense to increase mobility.
Medications play a vital role in managing the pain and inflammation associated with frozen shoulder. Common medications include Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), Pain killers or analgesic and oral corticosteroids. In some cases, a short course of oral corticosteroids may be prescribed to reduce inflammation and improve mobility in the shoulder.
Step 2: Interventional Injection
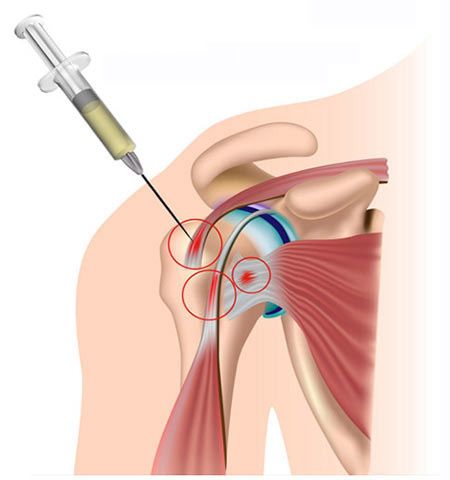
What make us difference from others is our doctors specialised training for injection under ultrasound guided towards the injured tissue. After thorough history taking and careful examination, most of the underlying injury in Frozen Shoulder can be identified. Depending on the type of injury, specific injection can be given under real-time ultrasound scan to ensure accuracy. Below are some of the common injections given for Frozen Shoulder:
1. Subacromial Subdeltoid Hydrodissection
This minimally invasive procedure involves the precise injection of fluid between the deltoid muscle and the shoulder joint’s subacromial bursa. The goal is to release adhesions and separate layers of tissue that have become stuck together due to inflammation. Hydrodissection helps to improve shoulder mobility and reduce pain by creating space for the tissues to move more freely.
2. Glenohumeral Joint Injection
The glenohumeral joint is the primary joint of the shoulder, where the head of the humerus fits into the socket of the scapula. A glenohumeral joint injection involves administering corticosteroids or hyaluronic acid directly into this joint. This treatment reduces inflammation, eases pain, and can significantly enhance the range of motion. It is particularly effective during the initial “freezing” stage of frozen shoulder.
3. Biceps Tendinitis Injection
In some cases of frozen shoulder, inflammation of the biceps tendon contributes to pain and restricted movement. A biceps tendinitis injection targets this specific area, delivering anti-inflammatory medication directly to the inflamed tendon. This injection reduces pain and allows for improved participation in physical therapy, aiding in the overall treatment of frozen shoulder.
4. Spinoglenoid or Suprascapular Nerve Block
Nerve blocks are used to manage severe pain associated with frozen shoulder. The spinoglenoid or suprascapular nerve block involves injecting a local anesthetic near the nerves that supply the shoulder. By blocking these nerves, the procedure can provide significant pain relief, allowing for more aggressive physical therapy and quicker recovery.
Step 3: Surgery

Surgery is typically considered when non-surgical treatments, including physical therapy, medications, and injections, have not provided sufficient relief after several months. The decision to proceed with surgery depends on the severity of the condition, the patient’s overall health, and their willingness to engage in post-operative rehabilitation.
Surgical intervention aims to release the tight, contracted tissues that restrict shoulder movement, providing long-term relief and restoring functionality.
1. Manipulation Under Anesthesia (MUA)
Manipulation under anesthesia is a procedure where the patient is placed under general anesthesia, and the surgeon carefully moves the shoulder through its range of motion. The goal is to break up the scar tissue and adhesions that have formed in the joint capsule, thereby increasing mobility. This procedure is typically followed by an intensive physical therapy regimen to maintain the improved range of motion.
2. Arthroscopic Capsular Release
Arthroscopic capsular release is a minimally invasive surgical technique that involves the use of a small camera (arthroscope) and specialized instruments to cut through the tight, thickened capsule of the shoulder joint. This procedure specifically targets areas of the capsule that are most restricted, allowing for a more customized release. Arthroscopic capsular release has the advantage of being less invasive than open surgery, with shorter recovery times and reduced risk of complications.
3. Open Surgical Release
In more severe cases of frozen shoulder, where arthroscopic techniques may not be sufficient, open surgical release might be required. This involves a larger incision to access the shoulder joint, allowing the surgeon to manually remove or release the scar tissue and adhesions. Open surgical release is generally reserved for cases that have not responded to other treatments, and while it is more invasive, it can be highly effective in restoring shoulder function.
